On Jan. 10, 2018, the Centers for Medicare & Medicaid Services (CMS) released a memo in which it announced that it will now review Medicare Advantage organizations’ networks on a three-year cycle — representing a significant change in operating procedure. For the first triennial review cycle, CMS will pull a sample of active contracts, including contracts that have not undergone a full network review since contract initiation. CMS will provide the selected organizations at least 60 days’ notice before the mid-June deadline to submit data on their networks.
How big of a deal is CMS’ network “crackdown”? While readiness varies by plan, a sampling analysis of Medicare Advantage plans’ published online provider directories indicates that many plans are not sufficiently prepared for a CMS network adequacy audit and could face a range of serious repercussions.
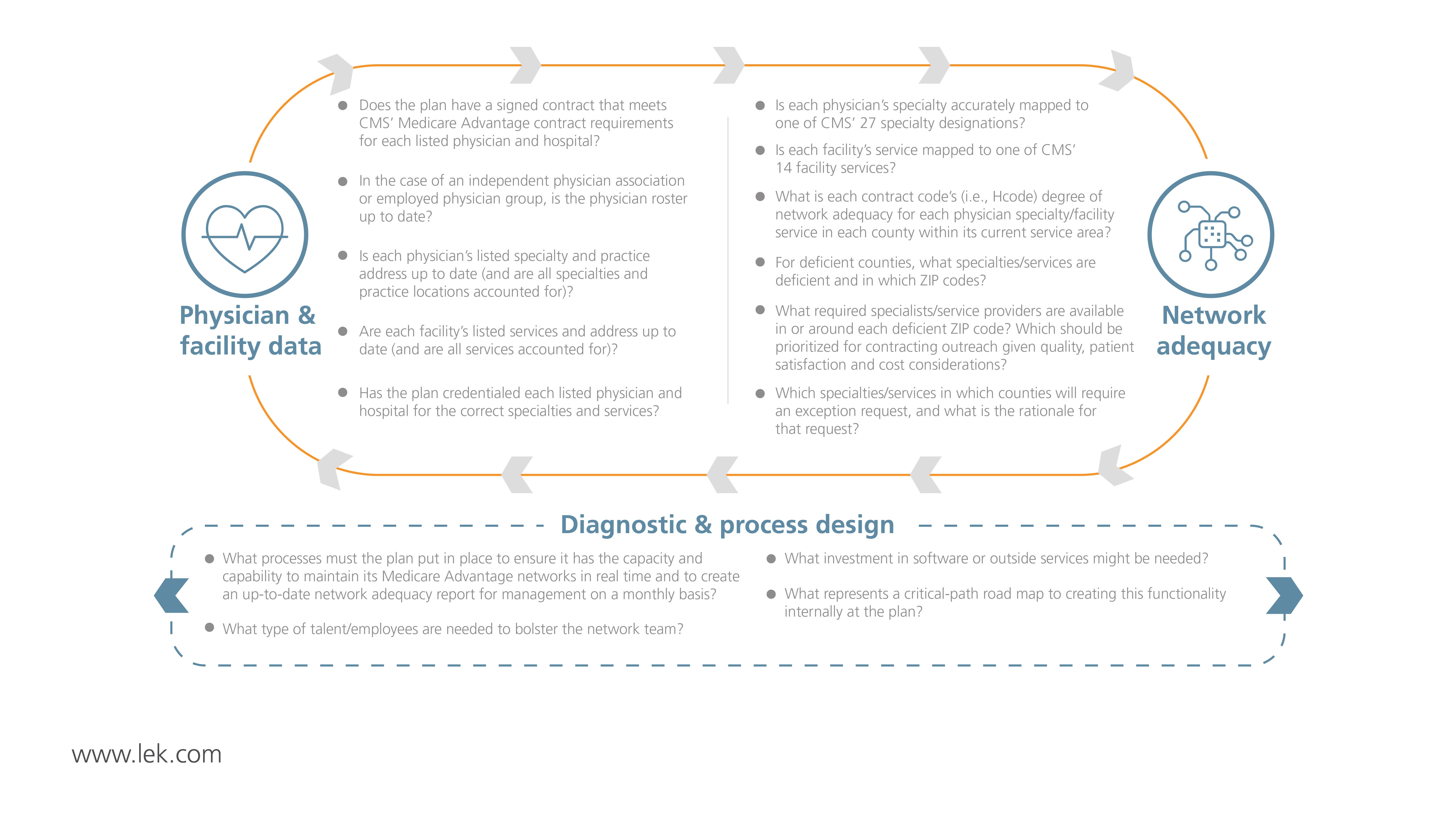
Our Healthcare Services Solutions explains the CMS’ “crackdown” and discusses its effect on Medicare Advantage plans. In addition, learn more about how L.E.K. Consulting can help to ensure plans are ready for and can react quickly to a CMS audit. We’ve conducted holistic provider network reviews for a host of Medicare Advantage clients and have developed a tried-and-true process to generate adequate and accurate HSD tables and approved exception requests.
Sample Visuals
04242019150422